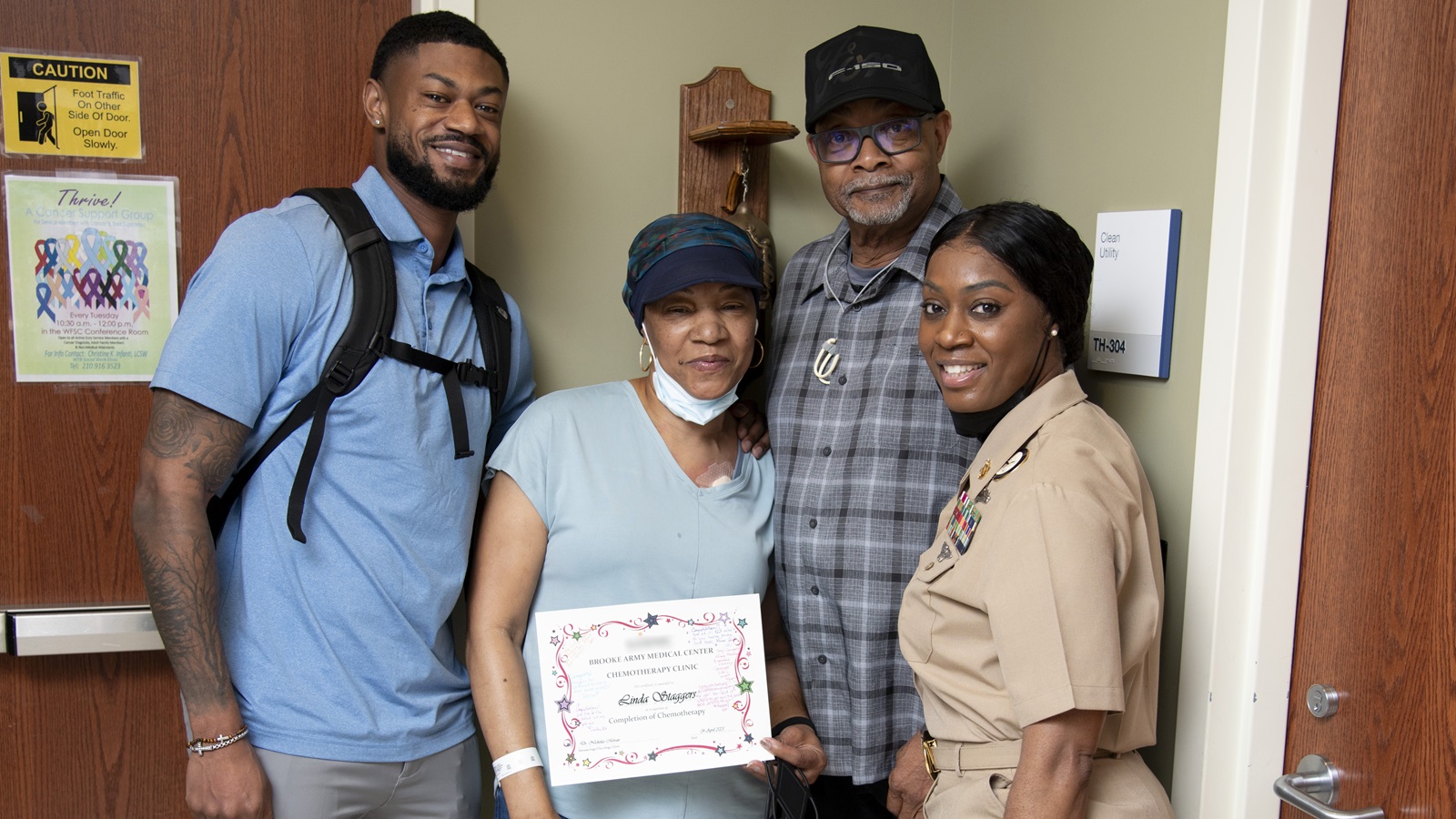
April 07, 2025 | By Lori Newman, Brooke Army Medical Center Public Affairs
JOINT BASE SAN ANTONIO-FORT SAM HOUSTON, Texas – Two Air Force neurologists at Brooke Army Medical Center specialize in movement disorders including Parkinson’s disease.
Parkinson's disease is a progressive neurologic disorder due to damage of neurons or brain cells. Patients experience symptoms as a result of the degeneration in the form of movement impairments including stiffness, slowness, tremor, imbalance.
According to the Parkinson’s Foundation, nearly one million people in the Unites States are living with Parkinson’s Disease. Parkinson’s is the second-most common neurodegenerative disease after Alzheimer’s disease. “Parkinson's disease is increasing at an exponential rate,” said Air Force Capt. (Dr.) William Hoffman, medical director of Joint Integrated Clinical Medicine, Office of Science and Technology, 59th Medical Wing. “It's the number two degenerative disease in the world.”
“Even though Parkinson’s is a neurodegenerative condition, like Alzheimer's, the key difference is that symptoms of Parkinson’s is highly treatable,” said Air Force Maj. (Dr.) Jessie Jacobson, neurologist. “We can treat a lot of the symptoms, essentially giving patients living with Parkinson's the ability to have a normal life.”
Hoffman and Jacobson are currently the only two Air Force neurologists who specialize in movement disorders. Additionally, there are only a few movement disorders specialists within the San Antonio community.
Parkinson’s Symptoms
According to the National Institute of Health, PD affects different people in different ways. The rate of progression and the particular symptoms differ among individuals. PD symptoms typically begin on one side of the body. However, the disease eventually affects both sides, although symptoms are often less severe on one side than on the other. The four primary symptoms of PD are:
- Tremor (shaking) which often begins in a person’s hand, although sometimes the person’s foot or jaw is affected first.
- Rigidity (muscle stiffness), or resistance to movement. The muscles stay tense and tight so the person aches or feels stiff.
- Bradykinesia, a slowing down of spontaneous and some automatic movement. It can make simple tasks more difficult, and activities the person could once perform quickly and easily—such as washing or dressing—may take much longer.
- Postural instability, such as balance problems and changes in posture, can increase the risk of falls.
Other symptoms can include mental and emotional health problems, difficulty swallowing or chewing, speech changes, urinary problems or constipation, skin and sleep problems, dementia, orthostatic hypotension, pain, fatigue, and sexual dysfunction.
Treatment Options Available
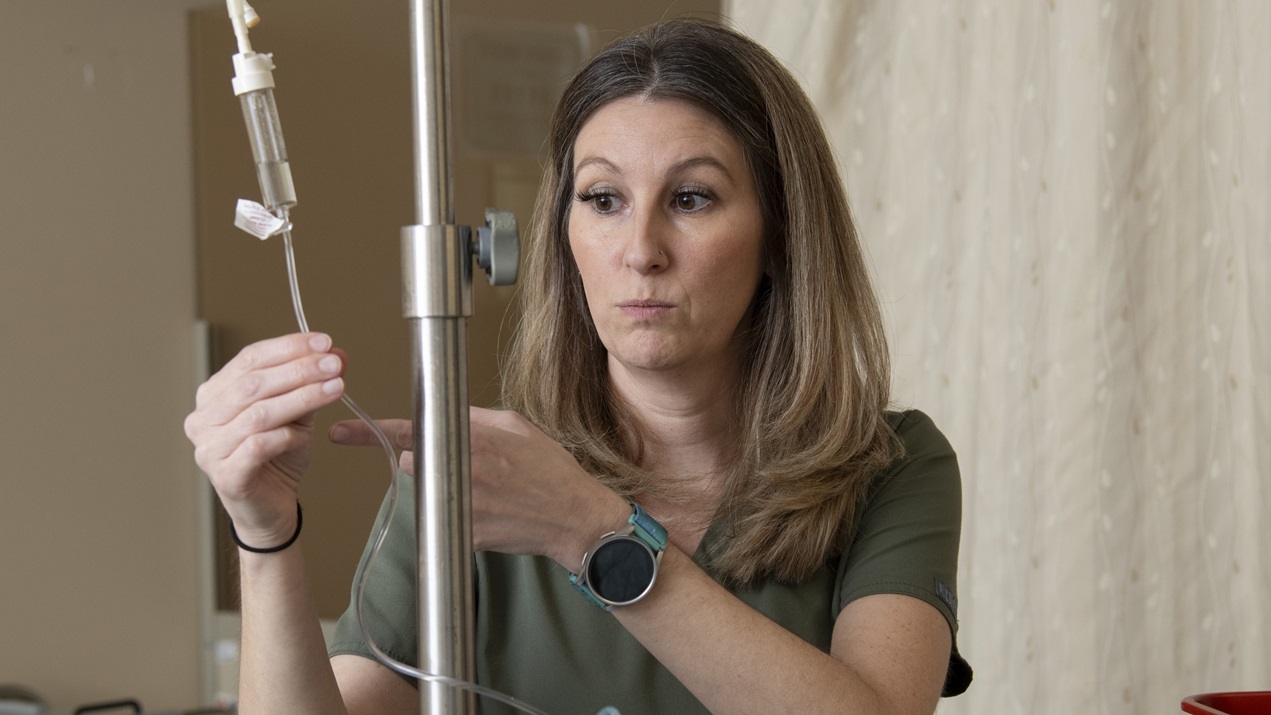
Currently, there is no cure for PD, but medications or surgery can improve many of the movement symptoms people experience. “Part of the treatment is through medications and the other half, really important as well, is through neuromodulation,” Jacobson said.
Neuromodulation is a therapeutic technique that involves altering the activity of the nervous system by delivering electrical stimulation to specific brain regions.
Deep brain stimulation is a surgical therapy used to treat certain aspects of Parkinson’s disease. This therapy addresses the movement symptoms of Parkinson’s and can help manage certain side effects caused by medications. “If you think about pacemaker for the heart, this is like pacemaker for the brain,” Jacobson explained.
During DBS surgery, electrodes are inserted into a targeted area of the brain and a second procedure is performed to implant an impulse generator battery (called an IPG), which is similar to a heart pacemaker and approximately the size of a stopwatch. The IPG is placed under the collarbone or in the abdomen and delivers an electrical stimulation to targeted areas in the brain that control movement through electrodes placed in the brain.
“Initially, during the first stages of the DBS programming, we will see the patient one month after surgery, then every 3-4 months in the first year to make sure everything is optimized,” Jacobson explained. “After that they can come back once or twice a year to get it checked. We have a tablet, which will tell us all the information about the patient's device and the patient has a little tablet themselves, that will show them the battery life.”
“With the tablet, I can do an analysis and see exactly what the brainwaves are and then we can target the simulation and steer it exactly to the brainwaves causing the symptoms,” Hoffman added. “The tricky thing is that not everyone is going to benefit from this. We’ve got to make sure the patient gets diagnosed and selected from neuromodulation properly.”
“There’s no blood test for Parkinson’s,” he added. “It’s all based on a clinical diagnosis. That’s why a referral to a movement specialist is so important.”
Research Study for Active-Duty Service Members
The average age of onset is in a person’s early to mid-60s, and the incidence rises significantly with older age. However, a small percentage of people with PD has “early-onset” Parkinson’s disease, which begins before the age of 50. “When we say early-onset, we mean people are getting Parkinson's in their 30s, 40s, 50s,” said Jacobson.
“In our clinic, we're seeing increasing numbers of active-duty patients with Parkinson's disease which is concerning,” Hoffman said. “To our knowledge, no one has actually researched early-onset Parkinson's disease in active-duty service members, but we know that this population has many of the risk factors of Parkinson's disease.”
Hoffman said some of those risk factors include head injuries, post-traumatic stress disorder and possible exposure to certain types of chemicals. “Our study aims to do a very detailed, comprehensive investigation of these patients,” Hoffman said. “We're going into their deployment history, where they've been stationed, their exposure history – testing for toxic exposures in their body. We'll do a range of other diagnostic tests; test their genetics and check their microbiome because certain types of gut bacteria changes are associated with the development of the disease.”
While the exact cause of PD is unknown, some cases are hereditary and can be traced to specific genetic mutations. Most cases are sporadic, meaning they arise with no known cause. However, researchers think that PD likely results from a combination of genetics and exposure to one or more (mostly unknown) environmental factors that trigger the disease.
“Studying these patients is important, because we need to figure out where the problem is so we can prevent it,” Hoffman added. “10% of people with Parkinson’s disease are primarily genetic, but the other 90% don’t have any identifiable genes. There’s so much we don’t know.”
“There is evolving evidence that toxic exposure and pollutants in our environment is likely a key driver for Parkinson’s disease around the globe,” Hoffman added. “I think we all have a vested interest in being informed about what we put in the environment and what we are putting into our bodies.”
The Bottom Line
The earlier someone gets diagnosed for Parkinson’s disease the better. “The timing of diagnosis is important because the sooner someone starts treatment, the more mobile, the more active they are, they can get their quality of life back,” said Jacobson. “We know exercise can potentially impact how the disease progresses. So that's why it's important to get diagnosed accurately and early and start the treatment.”
“It’s also important for people to stay active, both physically and socially,” she added. “Even if you cannot see a movement specialist, you can do that on your own now.”
TRICARE beneficiaries who are experiencing any of the symptoms of PD should talk with their primary care team to get a referral to the BAMC Neurology Clinic for evaluation.